What is Heart Failure?
Heart failure is a chronic condition characterized by the heart’s inability to pump blood effectively, resulting in inadequate blood flow to meet the body’s needs. This does not mean that the heart has completely stopped working; rather, it indicates that the heart’s pumping capacity has become compromised.
Heart failure can develop gradually over time or occur suddenly due to various factors. It may affect one side of the heart or both, leading to a range of symptoms that can significantly impact quality of life.
Definition of Heart Failure
Heart failure is defined as the heart’s inability to pump blood effectively, which leads to a decrease in the supply of oxygen and essential nutrients to the body’s tissues. This condition can manifest in various ways, with common symptoms including fatigue, shortness of breath, and fluid retention.
Importantly, heart failure is often a progressive condition, requiring ongoing management and treatment to improve the patient’s quality of life.
Types of Heart Failure
There are several types of heart failure, each with distinct characteristics. Systolic heart failure, also known as heart failure with reduced ejection fraction (HFrEF), occurs when the heart muscle becomes weakened and cannot contract effectively. This results in a reduced amount of blood being pumped out with each heartbeat.
In contrast, diastolic heart failure, or heart failure with preserved ejection fraction (HFpEF), occurs when the heart muscle becomes stiff and struggles to relax, preventing it from filling adequately with blood between beats.
Heart failure can also be categorized based on which side of the heart is affected. Right-sided heart failure typically results from left-sided heart failure and leads to fluid buildup in the body, particularly in the legs and abdomen.
Left-sided heart failure can manifest as either systolic or diastolic failure, primarily affecting the left side and causing fluid to back up into the lungs.
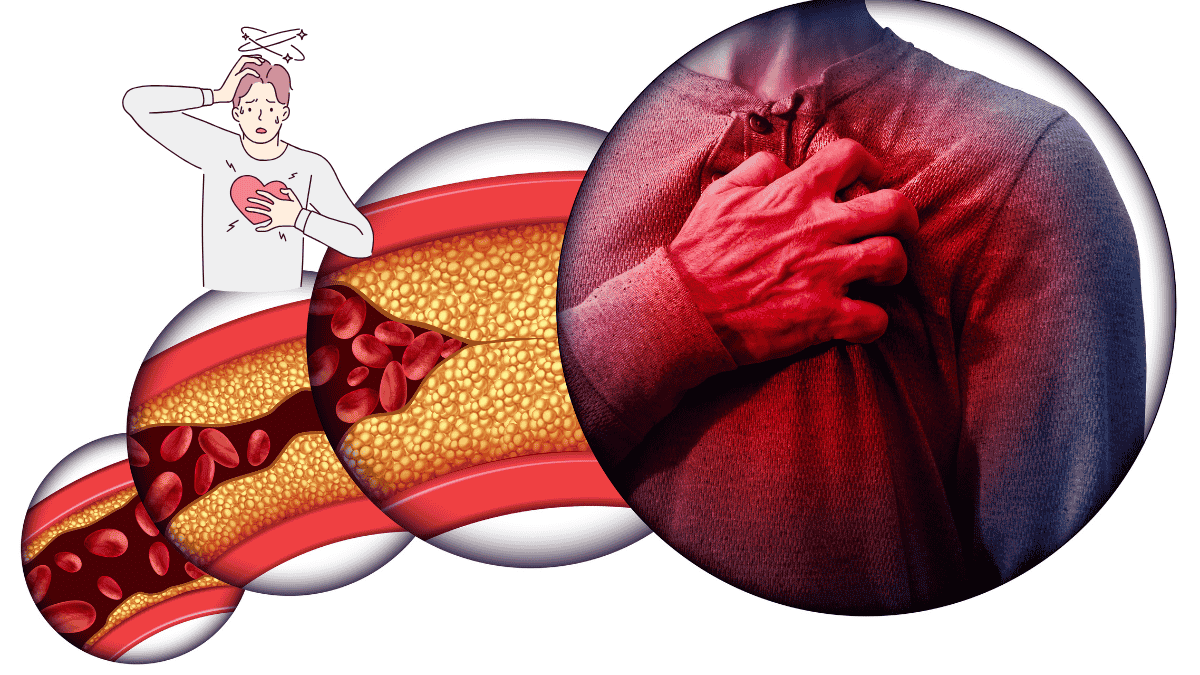
Symptoms of Heart Failure
Heart failure presents a variety of symptoms that can significantly impact daily life. Spotting these symptoms early is key to successful treatment and management.
Common Symptoms
The most common symptoms of heart failure include persistent fatigue and weakness, which can make everyday activities feel exhausting. Individuals often experience shortness of breath, especially during physical exertion or while lying down.
This can be accompanied by coughing or wheezing, particularly when fluid accumulates in the lungs.
Swelling, or edema, in the legs, ankles, or abdomen is also frequent, caused by fluid retention. Other symptoms may include a rapid or irregular heartbeat, difficulty concentrating, and a decreased ability to exercise or engage in physical activities.
Warning Signs to Watch For
In addition to common symptoms, there are specific warning signs that should prompt immediate medical attention. These include sudden weight gain due to fluid retention, pronounced shortness of breath at rest, or worsening symptoms after previously stable periods.
Chest pain or pressure, along with fainting or severe dizziness, are critical signs that may indicate a more serious issue. If these symptoms arise, it is vital to seek medical help promptly to prevent complications and ensure appropriate treatment.
Being aware of these warning signs can help individuals take proactive steps in managing their heart health.
Causes of Heart Failure
Heart failure can arise from various causes, often stemming from underlying health conditions that damage the heart or affect its ability to function effectively. Comprehending these causes is crucial for both prevention and effective management.
Risk Factors
Multiple risk factors can elevate the chances of developing heart failure. Age is a key factor, with the risk increasing as people get older. Other common risk factors include high blood pressure, which puts extra strain on the heart, and coronary artery disease, where the heart’s blood supply is reduced due to narrowed arteries.
Conditions such as diabetes and obesity are also critical risk factors, as they can lead to heart damage over time. Lifestyle choices, including smoking, excessive alcohol consumption, and a sedentary lifestyle, further contribute to the risk. Additionally, a family history of heart disease can increase an individual’s susceptibility to heart failure.
Underlying Conditions
Heart failure often develops as a result of underlying medical conditions that compromise heart function. These can include ischemic heart disease, which occurs when the heart’s blood supply is reduced, often due to blockages. Other conditions, such as cardiomyopathy, involve the deterioration of heart muscle, making it harder for the heart to pump effectively.
Hypertension, or chronic high blood pressure, is another major contributor, as it forces the heart to work harder over time. Additionally, heart valve disorders can disrupt normal blood flow, leading to heart failure.
Other contributing factors may include arrhythmias, thyroid disorders, and chronic lung diseases, which can all adversely affect the heart’s ability to function properly. Understanding these causes and conditions is vital for developing effective prevention and treatment strategies.
Diagnosis of Heart Failure
A precise diagnosis is essential for the effective management of heart failure. It involves a combination of clinical evaluation, medical history, and various diagnostic tests.
Diagnostic Tests
To diagnose heart failure, healthcare providers may employ several diagnostic tests. These typically include physical examinations to assess symptoms and vital signs. Imaging tests, such as echocardiograms, provide detailed pictures of the heart’s structure and function, allowing doctors to evaluate how well the heart is pumping.
Blood tests can also be conducted to measure levels of certain substances, such as natriuretic peptides, which can indicate heart strain. Additional tests, like chest X-rays, help identify fluid buildup in the lungs or other complications. In some cases, more advanced imaging, like MRI or CT scans, may be used for further assessment.
Importance of Early Detection

Early detection of heart failure is vital for improving outcomes and enhancing quality of life. Recognizing symptoms early allows for timely intervention, which can prevent the progression of the disease.
Additionally, identifying risk factors and underlying conditions can facilitate appropriate treatment plans and lifestyle modifications.
Early diagnosis also provides individuals with the opportunity to better manage their heart health, reducing the likelihood of severe complications and hospitalizations.
Treatment Options for Heart Failure
Managing heart failure involves a comprehensive approach that includes lifestyle changes, medications, and, in some cases, surgical interventions.
Lifestyle Changes
Adopting a heart-healthy lifestyle is foundational in managing heart failure. This includes following a balanced diet low in salt, saturated fats, and sugars to help control blood pressure and weight. Regular physical activity, tailored to individual capabilities, can strengthen the heart and improve overall well-being.
Additionally, quitting smoking and limiting alcohol intake are crucial steps in reducing heart strain. Patients are often encouraged to monitor their weight regularly to catch any sudden fluid retention early.
Medications
Various medications are prescribed to help manage heart failure symptoms and improve heart function. Common classes of medications include diuretics, which help reduce fluid buildup; ACE inhibitors and ARBs, which lower blood pressure and reduce strain on the heart; and beta-blockers, which slow the heart rate and improve heart efficiency.
Other medications, such as aldosterone antagonists, can also be beneficial. It’s important for patients to follow their prescribed medication regimen closely and consult their healthcare provider about any side effects or concerns.
Surgical Options
In some cases, surgical interventions may be necessary for heart failure management. Procedures can range from the implantation of devices, such as pacemakers or implantable cardioverter-defibrillators (ICDs), to more invasive surgeries like heart valve repair or replacement. In severe cases, heart transplantation may be considered when other treatments are ineffective.
These surgical options aim to improve heart function and enhance the quality of life for individuals living with heart failure. Regular follow-up with healthcare professionals is essential to monitor the effectiveness of treatments and make necessary adjustments.
Conclusion
Heart failure is a complex and multifaceted condition that requires careful management and a proactive approach to treatment. Understanding the symptoms, causes, and available diagnostic methods is essential for early detection, which can significantly improve outcomes and quality of life.
Effective management often involves a combination of lifestyle changes, medications, and, in some cases, surgical interventions. By adopting heart-healthy habits and working closely with healthcare professionals, individuals can better navigate the challenges of heart failure and enhance their overall well-being.
FAQ
What is heart failure?
Heart failure is a chronic condition where the heart cannot pump blood effectively.
What are the common symptoms of heart failure?
Common symptoms include fatigue, shortness of breath, and fluid retention.
What causes heart failure?
Heart failure can be caused by conditions like high blood pressure, coronary artery disease, and diabetes.
How is heart failure diagnosed?
Diagnosis typically involves physical exams, blood tests, and imaging tests like echocardiograms.
What treatment options are available for heart failure?
Treatment options include lifestyle changes, medications, and surgical interventions if necessary.


Pingback: Heart Murmur Causes, Symptoms, and Treatment Options